- With MdDS remission, do symptoms decrease gradually or disappear suddenly?
-
New members to our support groups often ask, “For those of you who went into remission, did your MdDS symptoms decrease gradually over time, or did they disappear suddenly?”
Generally, symptoms wane gradually. Some experience relief every other day with the number of good days increasing until there are no bad days.
- Are there similar conditions? What are some other balance disorders?
-
What is a balance disorder?
The National Institute on Deafness and Other Communication Disorders (NIDCD) defines a balance disorder as a condition that makes you feel unsteady or dizzy. If you are standing, sitting, or lying down, you might feel as if you are moving, spinning, or floating. If you are walking, you might suddenly feel as if you are tipping over. The NIDCD adds that there are more than a dozen different balance disorders. Here are just a few common balance disorders.
- Benign paroxysmal positional vertigo (BPPV) or positional vertigo: A brief, intense episode of vertigo triggered by a specific change in the position of the head. You might feel as if you’re spinning when you bend down to look under something, tilt your head to look up or over your shoulder, or roll over in bed. BPPV occurs when loose otoconia tumble into one of the semicircular canals and affect how the cupula works. This keeps the cupula from flexing properly, sending incorrect information about your head’s position to your brain, and causing vertigo. Read More.
- Labyrinthitis: An infection or inflammation of the inner ear that causes dizziness and loss of balance. It is often associated with an upper respiratory infection, such as the flu. Read More.
- Ménière’s disease: Episodes of vertigo, hearing loss, tinnitus (a ringing or buzzing in the ear), and a feeling of fullness in the ear. It may be associated with a change in fluid volume within parts of the labyrinth, but the cause or causes are still unknown. Read More.
- Vestibular neuronitis: An inflammation of the vestibular nerve that can be caused by a virus, and primarily causes vertigo. Read More.
- Perilymph fistula: A leakage of inner ear fluid into the middle ear. It causes unsteadiness that usually increases with activity, along with dizziness and nausea. Perilymph fistula can occur after a head injury, dramatic changes in air pressure (such as when scuba diving), physical exertion, ear surgery, or chronic ear infections. Some people are born with perilymph fistula. Read More.
- Persistent Postural-Perceptual Dizziness (PPPD): see diagnostic criteria established by the Bárany Society and International Headache Society. The document is available through the Journal of Vestibular Research.
- Vestibular Migraine: see diagnostic criteria established by the Bárany Society and International Headache Society. The document is available through the Journal of Vestibular Research.
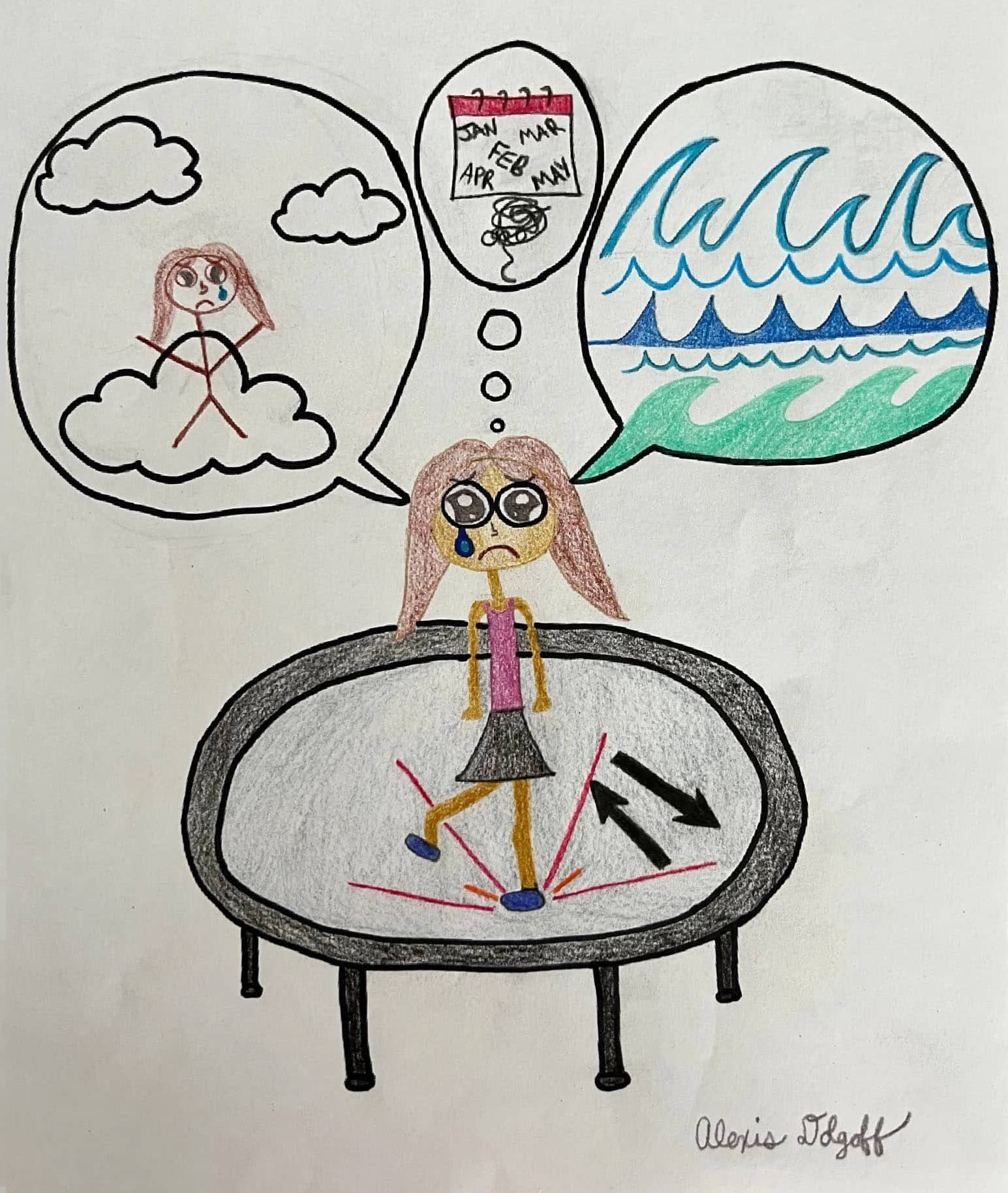
Other balance disorders may have symptoms in common with MdDS but, of note, symptoms of these conditions do not abate when the patient is in motion. A key diagnostic indicator of MdDS is that symptoms often temporarily remit when the patient is back in motion. When discussing your symptoms with your doctor, it is best to not use the words “dizzy” or “vertigo.” Instead, explain that you feel as if you are on a boat, walking on a trampoline or mattress, elevator drop, or other descriptive language.
Diagnostic Criteria for MdDS established by the Committee for the Classification of Vestibular Disorders of the Bárány Society can be found here: http://bit.ly/mddscriteria
What is vertigo?
Vertigo may be defined as a disorder of the sense of any direction, a disturbed spatial perception of the body, but vertigo usually means dizziness with spinning, a rotational sensation. And a frequent outcome when using the words “dizzy,” “dizziness” or “vertigo” when speaking with your doctor is a misdiagnosis with one of the above common balance disorders. A standard definition is being established by the Bárany Society of Neuro-Otology.
- How is MdDS Diagnosed?
-
Diagnostic Criteria for MdDS were published by the Bárány Society in 2020. The International Classification of Vestibular Disorders (ICVD) evidence-based consensus document can be found at http://bit.ly/mddscriteria.
Primarily diagnosed by an otolaryngologist or neurologist using patient history (e.g., recent travel or other motion experience) and by exclusion of other disorders, an MdDS diagnosis is usually not given unless a patient has experienced symptoms persisting for at least one month.
Presently there are no tests that can provide a definitive diagnosis of MdDS. Your doctor may order tests to eliminate other disorders which may have similar symptoms. A partial list of tests can be found on the Getting Diagnosed page of this website.
- What is MdDS?
-
MdDS is a central vestibular (neurological) disorder. It is not a peripheral vestibular (inner ear) disorder or disease. In the peer-reviewed research article, Metabolic and Functional Connectivity Changes in Mal de Debarquement Syndrome, author Yoon-Hee Cha, MD, et al discuss the areas of the brain associated with persistent MdDS.
What does MdDS stand for?
MdDS is the acronym for Mal de Débarquement Syndrome (Fr.), which translates to sickness upon disembarking (leaving a boat or other vehicle).
Is there an easier name than Mal de Débarquement Syndrome?
This disorder is also known as Disembarkment Syndrome, disembarkation syndrome, debarquement syndrome or colloquially as landsickness. It is less commonly known as Persistent Mal de Debarquement (PMdD), Rocking Dizziness or Rocking Vertigo.
- How did I get MdDS? I never went on a cruise. Can I have MdDS without a motion event?
-
Yes. While MdDS most often presents after a motion event (typically travel), about 20% of cases do not have a known causal event, i.e.: lack a motion trigger. A connection between spontaneous onset and migraine, stress, or other non-motion event has been suggested but further research is required to make any correlations.
Suggested Reading
Cha YH. Mal de Debarquement. Semin Neurol, 29:520-7, 2009. Review.
- How do I get an MdDS diagnosis? Should I see a GP or ENT?
-
MdDS is primarily diagnosed by otolaryngologists, ENTs and neurologists but can be diagnosed by your primary care provider. Other health professionals, including physical therapists and audiologists, may recognize the features of MdDS. You may wish to bring our informative brochure to your appointment as many health care providers are unaware of MdDS.
- Is there a cure for MdDS?
-
Unfortunately, no, but there are several on-going research studies.
You may be interested in the Physician’s Perspective blog post: Effective research requires teamwork.
- How do I prevent or reduce MdDS symptoms?
-
At present there are no treatments or therapies proven to be universally helpful to those suffering with MdDS. Some success in managing persistent symptoms has been realized with benzodiazepines, SNRIs, SSRIs and sometimes tricyclics. Vestibular rehabilitation therapy has shown effectiveness in a small number of patients, while a regular exercise program seems to help many.
Anticholinergic medications that work for typical forms of dizziness and motion sickness, such as meclizine or scopolamine, are not effective in either treatment or prevention of MdDS. Further research is required for a greater understanding of the disorder.
Investigative treatments are available but limited, usually requiring travel. To learn about treatments that sufferers have explored, you may wish to join one of our support groups.
- How long does MdDS last? I’m 2 weeks out from a cruise and am still on the boat.
-
How long does it take for MdDS to go away?
In most individuals, the sensation of rocking, bobbing, swaying, etc. following a cruise or other passive motion experience is transient. Symptoms lasting up to two weeks is considered within the normal range. A diagnosis of MdDS is usually only given to those whose symptoms last 30 days or more.
MdDS is often self-limiting, typically resolving within 4 months (median duration according to Cha et al, 2008).
MdDS may be episodic.
Patients in remission may experience recurring bouts, often associated with a precipitating event, e.g., travel or high stress. Subsequent episodes are generally more prolonged but some patients experience a quick return to baseline.
- Will symptoms worsen if I travel again?
-
Not necessarily. However, some individuals have described a transient increase in symptoms after further motion experiences. Some physicians suggest taking benzodiazepines to suppress the vestibular system during travel. While many patient members claim this course of action helps, clinical studies are required to prove their effectiveness across the population of MdDS sufferers.
- I have had MdDS that resolved on its own. Will I develop this again if I go on another cruise?
-
Some individuals who have had MdDS that resolved redeveloped symptoms after a subsequent cruise (or other prolonged motion experience, depending on their unique triggers). However, there are some who did not. Many describe a more prolonged period of MdDS symptoms with each episode. Therefore, the recommendation is to avoid further cruises to minimize the likelihood that MdDS will recur.
- Are MdDS symptoms worse during a woman’s period (menses)?
-
As with many chronic illnesses, many women experience increased symptoms before or during their menstrual cycle. While MdDS is more common in women than men, the role of hormones in the exacerbation/remission of MdDS symptoms is not understood.
- Are there any MdDS clinical trials/research studies?
-
Comprehensive information on MdDS clinical studies can be found on the National Institutes of Health (NIH) ClinicalTrials.gov website. Past research studies include one conducted at the University of Minnesota by Dr. Yoon-Hee Cha, and another at Ohio University by Dr. Brian C. Clark. Both of these studies were funded, in part, by this Foundation.